
May have tenderness directly over patella with characteristic radiographic findings Tenderness at patellar tendon insertion at inferior pole of patella in an adolescent Pain usually medial but poorly localized may have history of surgery Symptoms depend on origin of pain knee examination usually normal Referred pain from the lumbar spine or hip joint pathology
May be medial or lateral to patella if symptomatic, tenderness can be demonstrated on examinationĬharacteristic swelling anterior to patella following trauma Pain usually described as medial rather than anterior tenderness over pes anserine bursa May have crepitus or effusion characteristic radiographic findingsĪnterior knee pain “behind” or around patella usually no effusion may have findings of patellar maltracking Tenderness of tendon tendon may be thickened if chronic May have tenderness directly over patella Intermittent pain with sensation of instability or movement of patella may have swelling locking can occur with loose body formation may have tenderness over medial retinaculum Symptoms variable may have intermittent pain, swelling, or locking Tenderness and swelling at insertion of patellar tendon at tibial tubercle in an adolescent Symptoms variable may have intermittent sharp pain, locking, or effusion Typically presents with lateral pain and tenderness over lateral femoral epicondyle Pain and tenderness localized to infrapatellar fat pad Retropatellar pain may have history of trauma may have effusion on examination Pain may be insidious may have tenderness of bony structures May describe history of trauma mechanical symptoms may occur if loose body present may have effusion may have tenderness of involved structure (e.g., femoral condyles, patella) Educating patients about modification of risk factors is important in preventing recurrence. Surgery should be considered only after failure of a comprehensive rehabilitation program. There is little evidence to support the routine use of knee braces or nonsteroidal anti-inflammatory drugs. Recent research has shown that physical therapy is effective in treating PFPS.

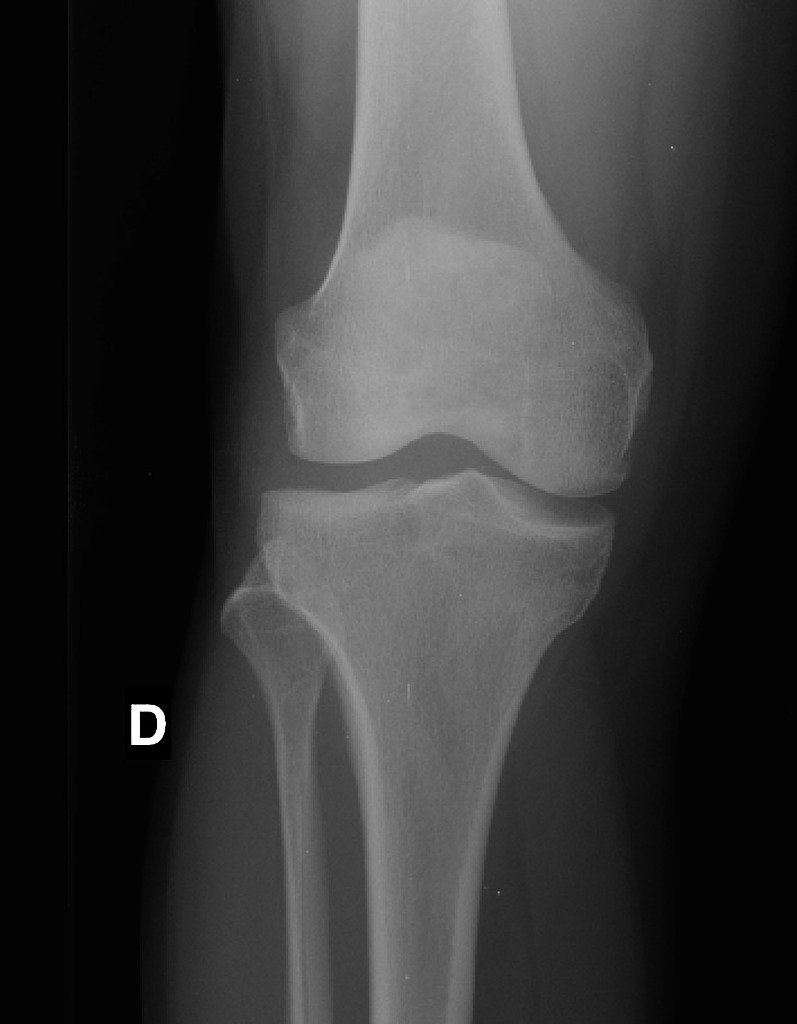
Radiography is recommended in patients with a history of trauma or surgery, those with an effusion, those older than 50 years (to rule out osteoarthritis), and those whose pain does not improve with treatment. For many patients with the clinical diagnosis of PFPS, imaging studies are not necessary before beginning treatment. To confirm the diagnosis, an examination of the knee focusing on the patella and surrounding structures is essential. Findings in patients with PFPS range from limited patellar mobility to a hypermobile patella. Typical symptoms include pain behind or around the patella that is increased with running and activities that involve knee flexion. Risk factors include overuse, trauma, muscle dysfunction, tight lateral restraints, patellar hypermobility, and poor quadriceps flexibility. It is caused by imbalances in the forces controlling patellar tracking during knee flexion and extension, particularly with overloading of the joint. Patellofemoral pain syndrome (PFPS) is the most common cause of knee pain in the outpatient setting.


 0 kommentar(er)
0 kommentar(er)
